October is Health Literacy Month: Do You Hear What I Hear?
October 24, 2017 • Uncategorized
College of Public Health & Texas Center for Health Disparities
Community Blog
Introduction
 My daughter, an Emergency Medical Technician (EMT), recently relayed a story about a call to which she responded. It involved an elderly couple in which the husband nearly killed his wife. How? Miscommunication, or a lack of health literacy. Healthcare miscommunication is the number one cause of medical error (AMA, 2007). The Institute of Medicine (IOM) defines health literacy as, “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions (IOM, 2004).” How do they do so, if health information is too hard to understand or people don’t have the capacity to understand (NAAL, n.d.)?
My daughter, an Emergency Medical Technician (EMT), recently relayed a story about a call to which she responded. It involved an elderly couple in which the husband nearly killed his wife. How? Miscommunication, or a lack of health literacy. Healthcare miscommunication is the number one cause of medical error (AMA, 2007). The Institute of Medicine (IOM) defines health literacy as, “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions (IOM, 2004).” How do they do so, if health information is too hard to understand or people don’t have the capacity to understand (NAAL, n.d.)?
 In this scenario, the wife was newly diagnosed with diabetes. The husband understood that giving her insulin would bring her blood sugars down but did not understand that the medicine needed to be balanced with food. Her sugars remained high so, he kept giving her insulin. She slipped into a diabetic coma…this is a patient safety issue. Thankfully, the MedStar responders explained to the couple how to balance the insulin with food.
In this scenario, the wife was newly diagnosed with diabetes. The husband understood that giving her insulin would bring her blood sugars down but did not understand that the medicine needed to be balanced with food. Her sugars remained high so, he kept giving her insulin. She slipped into a diabetic coma…this is a patient safety issue. Thankfully, the MedStar responders explained to the couple how to balance the insulin with food.
The Problem
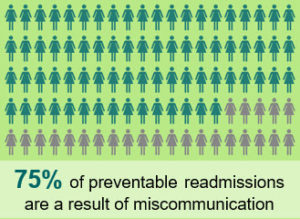
 Patients with poor health literacy may have increased readmissions, higher healthcare use, high healthcare costs and catastrophic outcomes (IOM, 2004). According to the Joint Commission on Accreditation of Hospitals, 75% of preventable readmissions are a result of miscommunication (DSHS, 2007). A nursing journal article by Dickens and Piano (2013), summarized the adverse health outcomes for people with low health literacy including higher emergency department use, medication errors, poor ability to manage chronic disease, less ability to recall healthcare information, higher rates of hospitalization with increased rates of readmission and higher rates of death.
Patients with poor health literacy may have increased readmissions, higher healthcare use, high healthcare costs and catastrophic outcomes (IOM, 2004). According to the Joint Commission on Accreditation of Hospitals, 75% of preventable readmissions are a result of miscommunication (DSHS, 2007). A nursing journal article by Dickens and Piano (2013), summarized the adverse health outcomes for people with low health literacy including higher emergency department use, medication errors, poor ability to manage chronic disease, less ability to recall healthcare information, higher rates of hospitalization with increased rates of readmission and higher rates of death.
The Solution
 The goals of Healthy People 2020 (2017) regarding health information include not only improving the health literacy of the population but also increasing the proportion of people who report that their healthcare providers have satisfactory communication skills. Improving health literacy can help providers deliver health information in a way that patients can understand and direct people to tools on the Internet and resources in the community to help them stay healthy and well or manage chronic disease (Nutbeam, 2000). According to the National Council on Aging, approximately 92% of older adults have at least one chronic disease, and 77% have at least two. Chronic diseases account for 75% of the money our nation spends on healthcare (NCOA, 2017).
The goals of Healthy People 2020 (2017) regarding health information include not only improving the health literacy of the population but also increasing the proportion of people who report that their healthcare providers have satisfactory communication skills. Improving health literacy can help providers deliver health information in a way that patients can understand and direct people to tools on the Internet and resources in the community to help them stay healthy and well or manage chronic disease (Nutbeam, 2000). According to the National Council on Aging, approximately 92% of older adults have at least one chronic disease, and 77% have at least two. Chronic diseases account for 75% of the money our nation spends on healthcare (NCOA, 2017).

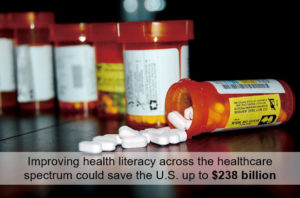
Improving health literacy across the healthcare spectrum and assisting with information usage could save the U.S. up to $238 billion annually (Vernon et al.,2007). In 2012, the IOM released a list of top 10 attributes of “health literate organizations.” This list provided standardized guidelines to address the complexity of modern healthcare as a barrier to health literate healthcare (IOM, 2012). As a result, health professional education has begun including health literacy as a part of their curriculum. Additionally, health literacy trainings effectively improve current practitioner’s health communication (Dickens et al., 2013; Nutbeam, 2000).
Call to Action
As a public health practitioner and resident of Tarrant County, I champion policy and programs to help everyone get simple health information to stay healthy and well. This includes working to help make healthcare easier to access and placing health education in K-12 schools. Thus, our children can grow up to be healthy adults. More recently, I have started a community collaborative to enable the sharing of resources and research among hospitals and community partners throughout our area. These efforts require “a village” to help improve the health and wellness of Tarrant County residents. If each resident asks questions when seeking healthcare to improve their understanding of health information and every healthcare and community organization embraces health literate care, we can work together towards a common goal. That goal: A community where all people receive easy to understand health information that promotes long, productive and healthy lives.
American Medical Association (AMA). (2007). Weiss, B. (ed.). Health Literacy and Patient Safety: Helping Patients Understand. Retrieved from: http://med.fsu.edu/userFiles/file/ahec_health_clinicians_manual.pdf
Department of State Health Services (DSHS). (2007). Texas Hospital Inpatient Discharge Public Use Data File Statistical Brief.
Dickens, C. & Piano, M. (2013). Health Literacy and Nursing: An Update. American Journal of Nursing, 113(6), 52-58.
Healthy People 2020 Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/health-communication-and-health-information-technology/objectives?topicId=18
Institute of Medicine (IOM). (2012). Attributes of a Health Literate Organization.
Brach, C. (Ed.). Retrieved from:
Institute of Medicine. (2004). Health Literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press.
National Assessment of Adult Literacy. (n.d.). NAAL factsheets: Health literacy component. Retrieved on March 31, 2009, from http://165.224.221.98/NAAL/fct_hlthliteracy.asp
National Council on Aging (NCOA). (2017). Healthy Aging Facts. Retrieved October 2017 from https://www.ncoa.org/news/resources-for-reporters/get-the-facts/healthy-aging-facts/
Nutbeam, D. (2000). Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 15(3), 259.
U.S. Department of State Health Services (USDSHS). (2017). Fact Sheet: Health Literacy and Health Outcomes. Retrieved from: https://health.gov/communication/literacy/quickguide/factsliteracy.htm
Vernon, J.A., Trujillo, A., Rosenbaum, S., & DeBuono B. (2007). Low Health Literacy: Implications for National Health Policy. Retrieved from http://publichealth.gwu.edu/departments/healthpolicy/CHPR/downloads/LowHealthLiteracyReport10_4_07.pdf
In peer reviewed research, low health literacy has been linked to poor outcomes:
|
Research reported in this publication was supported by the National Institute On Minority Health And Health Disparities of the National Institutes of Health under Award Number U54MD006882. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.


Social media