An Almost Forgotten but Still Important Health Risk: Tuberculosis
January 14, 2019 • Uncategorized
College of Public Health & Texas Center for Health Disparities Community Blog
Public Health Irony
An irony of public health is that the more effective we are the less visible we become—we work to prevent disease, to keep bad things from happening.
The constant chatter in social media isn’t focused on what isn’t happening in society, but on what is happening. Prevention isn’t flashy, it isn’t dramatic, and as a result there is little or no focus on much of what public health professionals and researchers really do. It’s easy to recognize and count things that happen; we track life expectancy and infant mortality and flu cases every day. In prevention, our success is measured by what doesn’t happen. Therefore, it can be easy to lose sight of the importance of these health protections.
UNTHSC’s College of Public Health works very hard to make sure we don’t lose sight of an almost forgotten but still critically important US health risk—tuberculosis (TB).
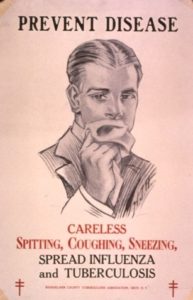
 History
History
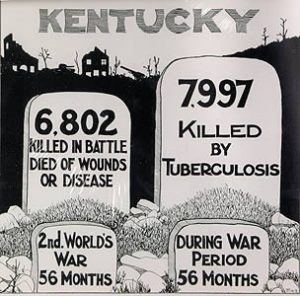
The slow-moving plague of TB has been part of the human experience longer than civilization, and until relatively recently there were few people in the US who were not affected by TB in some way. Before effective treatments and successful public health campaigns, the deadly threat of TB was just something people lived with daily, much like we still live with the ever-present risk of injury or death in a car accident.
In fact, the entire unincorporated city of TB patients and staff, called Sanatorium, Texas, came into existince due to the large number of Texans with active TB in the early 20th century. More formally known as the Texas State Tuberculosis Sanatorium, the city sprang up in Tom Green County near San Angelo in 1911, and many, many Texans lived and died there during the ensuing decades. My own family has a history with Sanatorium, and my great aunt died there in 1921 at age 19. By 1949, Sanatorium was home to over 1000 people, with it’s own power plant, elementary school, hog farm, dairy, library, post office and (!) the Chaser, it’s own newspaper. Sanatorium eventually dissolved with the advent of antibiotics and the post office officially closed in 1965.

The antibiotic era turned the tide band ushered in a period of steady progress toward TB control in the U.S. But TB remains a daily reality in much of the world. Even two decades into the 21st Century more people die of TB than any other infectious disease. In 2017, 10 million people became sick with TB, and 1.3 million died.
Today’s Efforts
My research colleague, Erica Stockbridge, as well as other UNTHSC and CPH colleagues, and I have been a part of US TB elimination efforts for many years. We are proud of what we have accomplished to improve public health. Just in the last decade our work has cut TB incidence in Tarrant County in half, driven other gains across Texas and the US, and established the standard of care for TB treatment internationally. Just as importantly, our research has contributed compelling justification for policymakers to continue providing critical support for the TB protections that have kept the US an island of safety in a sea of danger.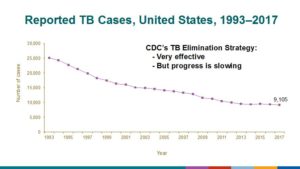
Over the years, continued efforts to eradicate TB have taken me to many of the places where it remains a daily reality. I have seen first-hand the suffering that comes without a strong and effective public health system. Disease doesn’t respect borders. Really, all that stands between our grandparents’ past and much of the world’s present is the diligent work by local, state, and national public health agencies to control and prevent TB in the US.
Are You At Risk of Developing TB?
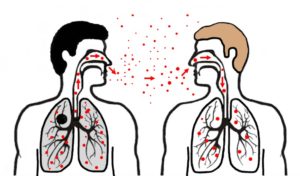
People can be infected with the bacteria that causes TB but have no symptoms and be unable to pass the disease to others. However, over time, 5-10% of these people with “sleeping,” latent TB infection will become sick with dangerous, active TB disease that can be passed to family and others. This progression from latent to active TB is preventable with treatment, though.
Up to 13 million people in the US have latent TB infection, and most future cases of TB disease in the US will occur in this group. This means that the best way to protect yourself against TB is to 1) determine if you are at-risk, 2) get tested for latent TB infection by your primary care provider or your local health department if you are at-risk, and 3) take and complete your medication regimen if you test positive and are a good candidate for treatment.
Ask your primary care provider about your risk of latent or active TB. People who are most at-risk include those who:
- Were exposed to someone who was sick with active TB
- Were born in a country where TB is common
- Have spent a month or more in a country where TB is common
- Are residents or employees of institutional residential facilities (e.g., prisons, homeless shelters)
- Have HIV infection
- Are taking medications that suppress the immune system (e.g., TNF alpha inhibitors such as adalimubab, infiximab or etanercept; organ transplant medication; long-term steroids; current cancer chemotherapy)
- Have leukemia or lymphoma
Authors
Erica Stockbridge, PhD, MA
If you are a health care provider, you can learn more about TB and latent TB infection by visiting the CDC website: (https://www.cdc.gov/tb/publications/ltbi/pdf/targetedltbi.pdf) and the US Preventive Services Task Force website: (https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/latent-tuberculosis-infection-screening) and reading recent literature reviews on the topic: (https://www.mdedge.com/jfponline/article/102196/infectious-diseases/tuberculosis-testing-which-patients-which-test).
Research reported in this publication was supported by the National Institute On Minority Health And Health Disparities of the National Institutes of Health under Award Number U54MD006882. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.


Social media